This week (December 6 through 12) is National Influenza Vaccination Week! Here to answer common questions about the flu vaccine is Lindsay Clarke, the Alliance’s Vice President of Health Education of Advocacy:
How serious can the flu be?
The seriousness of an influenza infection—more commonly called the flu—largely depends on age and the presence of other health conditions. People who are young and otherwise healthy are likely to recover in a few days to less than two weeks without any serious complications. But they still miss an average of six days of work and are often unable to care for their families or deal with other responsibilities. And even if their symptoms are mild, they are still contagious and can get other people sick—including people who might be more vulnerable to serious complications.
Infants, people with weakened immune systems, people from racial and ethnic minority groups, and older adults are all at higher risk of potentially serious complications from the flu—including hospitalization and death. Each year flu infections send hundreds of thousands of people to the hospital and cause tens of thousands of deaths from related pneumonia, sepsis, organ failure, heart attack, and more. The raised risk of heart attack is particularly alarming—with risk going up six times within a week of a confirmed flu infection—even in people who don’t have a history of heart disease.
Older adults are at an especially high risk because as we age, our immune systems decline and aren’t able to mount as strong a response to infections. Additionally, we are more likely to have chronic diseases that make it harder for our bodies to fight off infections and the complications that come with them.
Why do I need the flu vaccine every year?
Like most viruses, the influenza virus is constantly mutating and changing. This means that the strains of the virus that are being passed around from person to person change each year. Vaccine manufacturers produce new vaccines to give our body defenses against the strains of the virus that are known to be circulating in the community, so we need to get a new vaccine at the start of each cold and flu season in September and October.
Also, our immunity from the vaccine does decrease, or wane, over time so it’s important to give our immune systems an update each year.
I’ve already gotten the COVID-19 vaccine. Why do I need to get the flu vaccine on top of that?
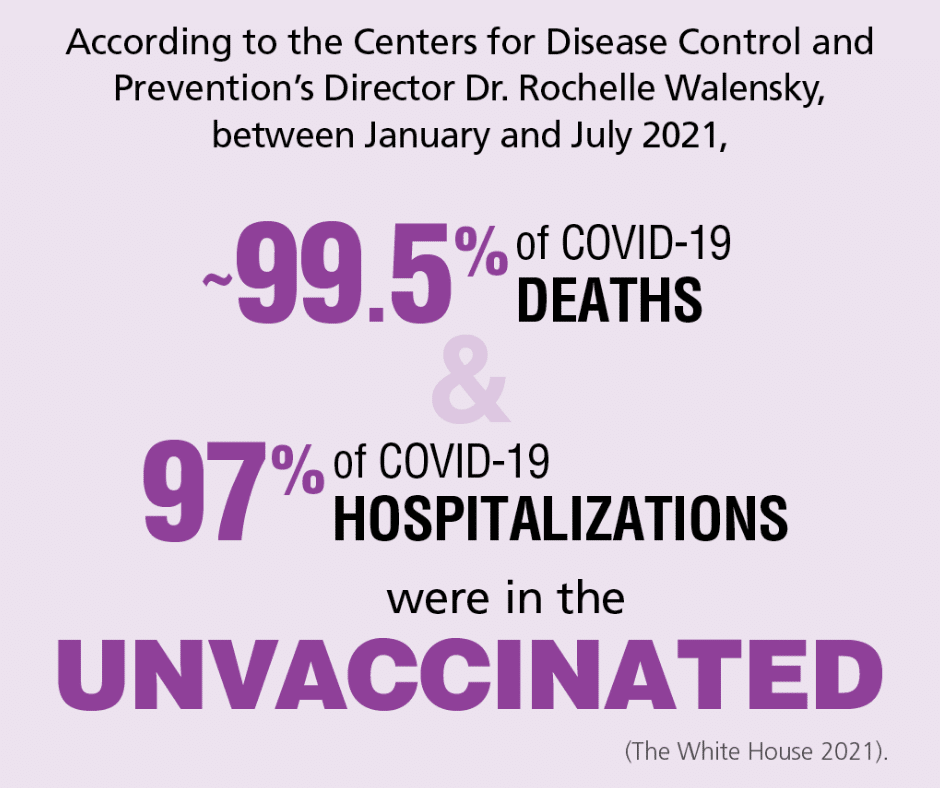
That’s great that you got your COVID-19 vaccine! The more people who are vaccinated, the fewer chances the virus has to spread. Plus, they are highly effective at reducing your risk of hospitalization and death from the virus.
But you still need a flu vaccine. Influenza and COVID-19 are different diseases caused by different viruses. Vaccines are developed to fight specific viruses, so they won’t protect you against other infectious diseases.
Can I get the COVID-19 vaccine or booster and the flu shot at the same time?
It’s safe to get your COVID-19 vaccine or booster and your flu vaccine at the same time—so while you’re scheduling one, you can go ahead and schedule the other. You may be concerned about possible side effects from the vaccines, but they shouldn’t be different than if you got the vaccines at separate times.
Are there any side effects to the flu vaccine?
The flu vaccine can cause arm soreness, muscle aches, and fatigue in some people. Side effects are generally mild and go away on their own. Severe side effects are rare, and despite what you may have heard, the flu vaccine can’t give you the flu. If you feel a little under the weather after your vaccine, this indicates that it’s working and causing your body to build up protection. And remember, it would likely be much worse if you got the actual flu.
Will I still get the flu if I get the vaccine?
The effectiveness of the flu vaccine varies from year to year and is never 100% effective at preventing illness. However, those who get the flu vaccine and still get the flu usually have milder symptoms, lower risk of complications, and a faster recovery. And every year the vaccines keep millions of people from getting the flu, prevent tens of thousands of hospitalizations, and save thousands of lives.
In addition to getting the vaccine, how can I help prevent the spread of the flu?
Getting a vaccine is your best defense against the flu, but you can also prevent the spread of the virus by handwashing, covering coughs and sneezes, and avoiding others when you’re sick.
Why do I need a high-dose or adjuvanted flu vaccine if I’m 65 or older?
As we age, our immune systems weaken and have trouble mounting the same defenses as when we were younger. Our bodies also don’t build up protection from vaccines like they used to. The high-dose and adjuvanted flu vaccines can help. The high-dose vaccine contains four times the dose of a regular flu vaccine, causing a better immune response than a regular dose. Adjuvanted flu vaccines include ingredients that help create a stronger immune response. So, be sure to talk to your healthcare provider about whether a high-dose or adjuvanted flu vaccine is right for you.
What are some warning signs of the flu?
Symptoms of the flu can vary from person to person but often include fever, chills, sweating, muscle aches, cough, congestion, runny nose, sneezing headaches, fatigue, loss of appetite, shortness of breath, sore threat, and swollen lymph nodes.
I’m feeling sick. How do I know if it’s COVID-19 or the flu?
It can be hard to tell on our own if you’re experiencing symptoms of the flu, COVID-19, a cold, RSV (respiratory syncytial virus), or something else since the symptoms are often similar. There are at home tests for COVID-19 and the flu—including combination tests that test for both at the same time. You can also go to your healthcare provider for tests. It’s important to figure out what you have so that you can isolate and inform any close contacts who may be infected. Your healthcare provider can also discuss treatment options including antivirals for the flu which can help reduce the severity of your illness. To date, one antiviral is also currently approved by the U.S. Food & Drug Administration (FDA) for use in patients 12 years of age and older for the treatment of COVID-19. Additionally, three monoclonal antibodies have been authorized for emergency use by the FDA. These monoclonal antibodies mimic the function of our immune system to help fight COVID-19 by blocking the ability of COVID-19 to attach and enter human cells and/or helping to clear cells which are already infected.