How would you feel about starting a race with no finish line? Or running in a race, only to find that the finish line is continually being moved back, leaving you with no idea of how long or how far you will have to run? Chances are you would cry “foul!”
That’s the situation faced right now by the developers of new drugs or medical technology, hoping to secure coverage for their products for patients on Medicare. The current “race with no finish line” is called the Coverage with Evidence Development Program (CED) and is used by the Centers for Medicare and Medicaid Services (CMS) to justify coverage decisions for the Medicare program. While the public reporting of health outcomes data and evidence-based shared decision-making tools such as CED are important and valuable, there needs to be a clear path – beginning, middle and end – for the process. Otherwise there is a chance that medical innovation will slow, and patients will be deprived of important, potentially life-saving, treatments.
When developing a new drug or medical technology, developers first focus on getting the evidence they need to achieve regulatory clearance from the Food and Drug Administration (FDA). Payers such as CMS sometimes need a different set of information to determine if the new drug or technology is medically necessary and beneficial to the population they serve. CED is intended to be used when there is some evidence of medical benefit, but more data are needed before a coverage decision can be made.
Transcatheter Aortic Valve Replacement
Last Friday, CMS issued its policy further extending the CED limitations for Transcatheter Aortic Valve Replacement (TAVR) for the treatment of symptomatic aortic valve stenosis for adults who need an aortic valve replaced. [Decision found here.] It was approved in 2011 by the FDA but due to concerns that such a new technology had risks, CMS imposed CED requiring that patients receiving TAVR are enrolled in prospective clinical studies or that additional data is collected through a patient registry intended to be used as the basis for future coverage decisions. CMS’ coverage decision went even further and required a doubling of the minimum number of annual surgical and/or interventional cardiac procedures for heart teams and hospitals to maintain a TAVR program.
To date, more than 200,000 thousand patients have been successfully treated with this therapy and dozens of studies have been published comparing TAVR to traditional open-heart surgery. These studies have shown positive results such as shorter hospital stays and recovery times, better quality of life measures, and lower incidences of some major complications. One would think that the positive results from these studies would show CMS that a Coverage with Evidence Development (CED) is no longer needed.
Unfortunately, that is not the case. CMS’ decision on Friday moved the finish line again for Medicare coverage for TAVR, mandating that it will remain available only through the CED program.
PET Amyloid Scans
Every year, thousands of Americans hear the devastating news that they have Alzheimer’s disease. This diagnosis carries with it a certain future of declining mental and behavioral capabilities, and the eventual need for round-the-clock end-of-life care. The financial costs can be staggering, and the emotional costs immeasurable. While the impact of Alzheimer’s can be slowed, the disease itself cannot be prevented. But some of the anguish surrounding the specter of this condition is entirely avoidable.
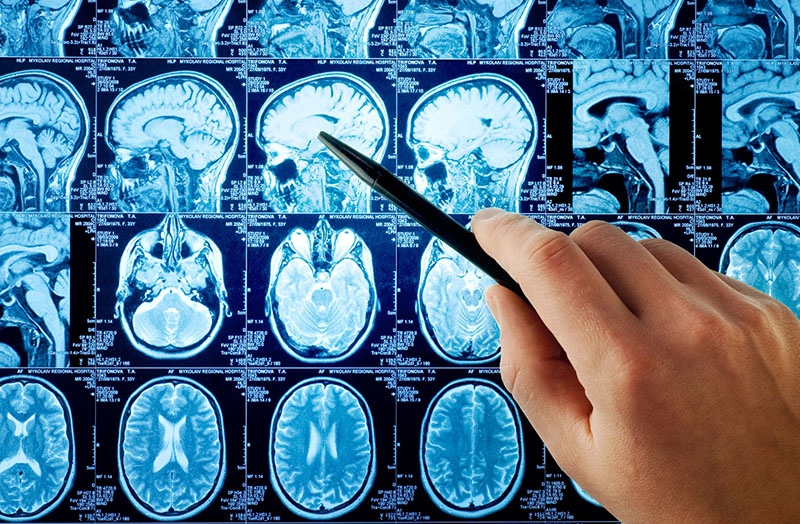
Positron-emission tomography (PET) imaging has been shown to detect the presence of amyloid plaques in the brain, one of the hallmarks of the disease, and similarly show their absence. Results from a new study published in the April 2, 2019 issue of the Journal of the American Medical Association shows that Imaging Dementia-Evidence for Amyloid Scanning (IDEAS) can have a significant impact on how patients with Alzheimer’s disease and other cognitive decline issues are diagnosed and treated.
Among the 11,409 Medicare beneficiaries with mild cognitive impairment or dementia of uncertain etiology evaluated by dementia specialists as part of the study it was found that the use of amyloid PET was associated with changes in clinical management within 90 days. The most recent results from the IDEAS study showed that physicians “changed their clinical management of more than 60 percent of patients in the study, more than double the number the authors had predicted in advance.”
CMS required that this study be conducted under its Coverage for Evidence Development Program to show value of PET amyloid scans for people with Medicare. It is time for CMS to recognize the compelling evidence from the study and reimburse broader use of the amyloid scans. People with Medicare are entitled to the accurate diagnosis of medical conditions that they may have based on their symptoms. Undoubtedly, the IDEAS trial results have already shown that PET amyloid scans are a useful aid to more accurate diagnosis. From a human suffering point of view, it could mean that thousands of individuals would avoid the angst of an incorrect Alzheimer’s diagnosis, and receive precise and effective medication for a potentially more treatable condition.
The CED program provides valuable data, and an extra level of security for American patients and their doctors. But the program needs to provide participants with clearly defined objective, and an equally as clearly defined schedule. No one wants to run a race with no finish line in sight.
Jim Scott serves as the chair of the Alliance for Aging Research’s Board of Directors. He is also the president and CEO at Applied Policy in Washington, D.C.