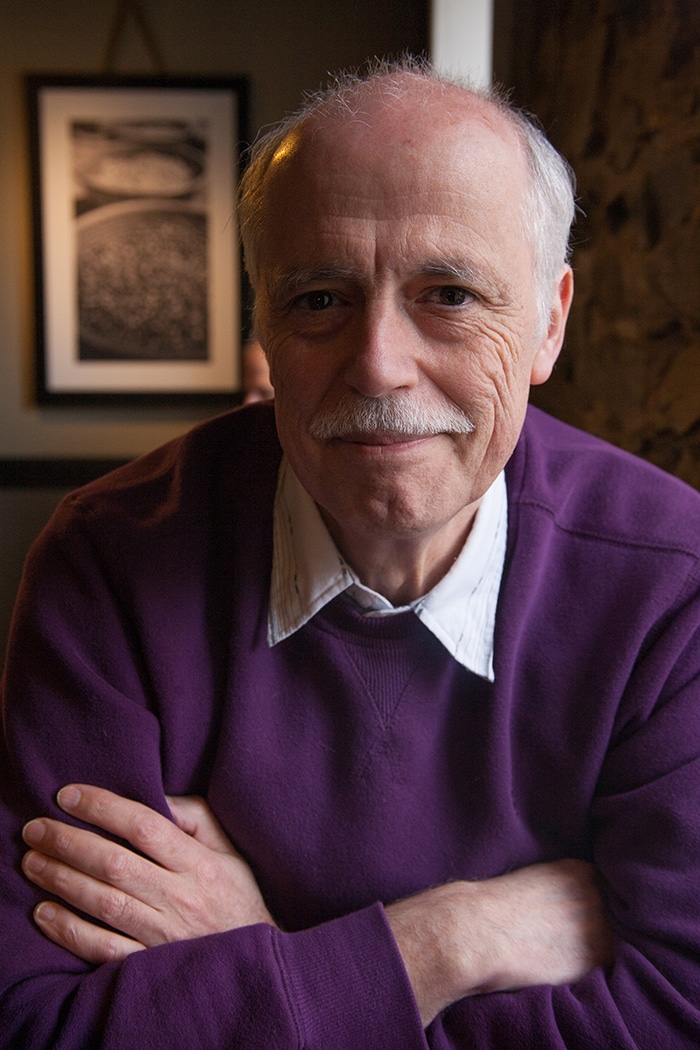
For this edition of the Healthspan Expert Q & A, we talk with Todd T. Brown, M.D., Ph.D., associate professor of Medicine and Epidemiology, Division of Endocrinology, Diabetes, and Metabolism, Johns Hopkins University, about HIV and how it affects the healthspan of older adults. We also discuss his research.
Q: Could you please tell us more about your background as a researcher?
TB: I’m an endocrinologist who has been working in the area of metabolic and endocrine abnormalities in HIV-infected persons for the past 15 years. My areas of interest are hypogonadism, osteoporosis, diabetes, and body composition changes in HIV infection, particularly as they relate to aging-related outcomes such as frailty and cardiovascular disease.
Q: How does HIV affect older adults, especially in comparison to other demographic groups?
TB: In general, the pathogenesis of comorbidities in HIV-infected persons is a complicated interaction of chronic inflammation due to HIV itself, antiretroviral medications, and risk factors leading to end-organ disease, such as behaviors (smoking, drug use) and co-infection (e.g. hepatitis C, CMV). These comorbidities also increase in frequency with aging, so what we’re seeing in older HIV patients is a confluence of the effects of aging and the impact of chronic HIV infection, antiretroviral therapy, and other risk factors. Antiretroviral therapy is very effective, so life expectancy in older HIV-infected persons is approaching that of their HIV-uninfected peers, but there is still a gap that needs to be better understood.
Q: What are researchers learning from studying HIV and how it relates to aging?
TB: Chronic inflammation is central to both aging and the pathogenesis of comorbidities in HIV-infected persons. In this way, chronic-treated HIV infection may help us understand the aging process in general.
Q: How are these discoveries benefiting patients right now? And what are some potential benefits from this research?
TB: Increased patient and provider awareness of the importance of screening for comorbidities such as diabetes, hypertension, dyslipidemia, osteoporosis, behavioral interventions (e.g., smoking cessation, weight reduction, exercise), and control of risk factors are critical steps in reducing the burden of aging-related diseases. Understanding the effect of antiretroviral therapies and developing strategies to optimize ART have also been an important product of aging-related research focused on HIV. Finally, there’s a lot of interest in finding therapeutic interventions to reduce the burden of immune activation and inflammation. There are many ongoing studies currently that may show promise for translation into the clinic.
Q: Can you tell us more about the 7th International Workshop on HIV & Aging on September 27 and 28 in Washington, D.C?
TB: This is a superb setting for investigators to showcase their cutting-edge research in the area of HIV and Aging. It’s a small, but very high-quality, abstract-driven meeting that fosters excellent discussion between participants and offers networking opportunities, especially for young investigators. For the plenary sessions, we try to get leading experts outside of HIV to bring insights from the general population to help us understand what we’re seeing in older HIV-infected individuals. We also have roundtable discussions and a hot topic debate. This year, the debate is about the pros and cons of testosterone replacement in the older adult.
Q: In your view, what is the ultimate goal of your research, and aging research in general?
TB: The overall goal is to optimize lifespan and healthspan in older HIV-infected persons. It’s a complicated field of science, but I think we’re making progress.