Roundtable Highlights Common Goals, Areas for Future Focus in Implementing Medicare Out-of-Pocket Cost Reforms
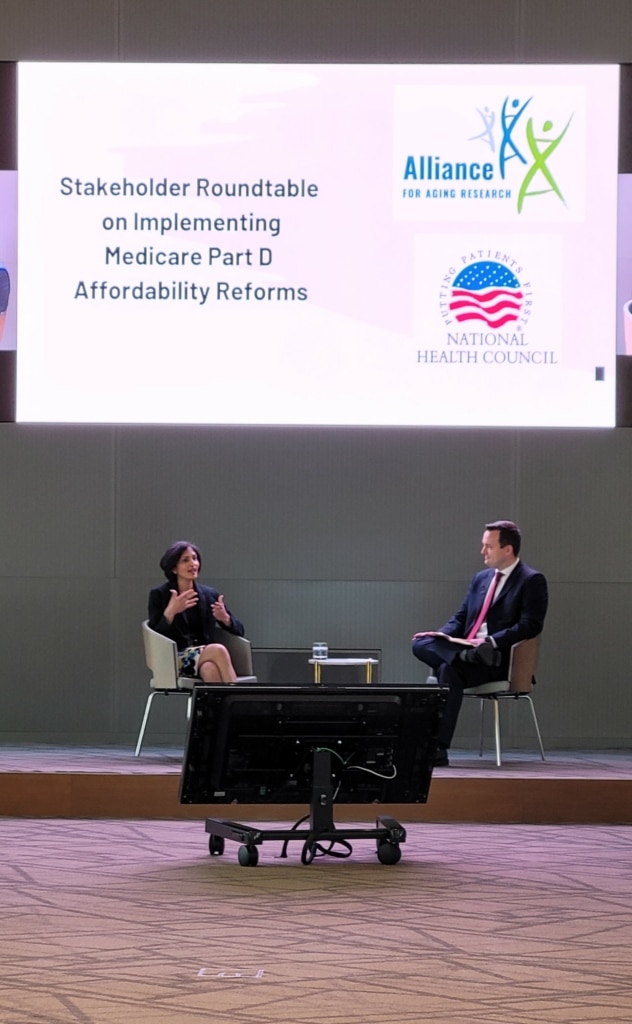
On May 2, 2023, the Alliance for Aging Research and the National Health Council brought together stakeholders including insurers, pharmacies, patient advocacy groups, and manufacturers for an open discussion about the upcoming changes to the Medicare Part D program passed in the 2022 Inflation Reduction Act. These changes, including the 1) introduction of a cost “smoothing” mechanism, enabling beneficiaries to pay their out-of-pocket (OOP) drug costs in monthly installments without interest, starting in 2025, and 2) implementation of a cap on annual OOP drug costs at $2,000, also commencing in 2025, were championed by patient advocates including the Alliance’s Project LOOP initiative.
While these two provisions offer the promise of helping Medicare beneficiaries to better afford their prescription medicines, there are many details that the law leaves up to the Centers for Medicare and Medicaid Services (CMS) to establish. These specifics include when beneficiaries will be able to decide to start using payment installments and the avenues that patients will receive information about the new benefits.
The participating organizations developed 11 recommendations for the Centers for Medicare and Medicaid Services (CMS) to consider while executing these changes. These recommendations are outlined in a summary of the roundtable discussions.
The recommendations underscore the importance of establishing clear and universally understood terminology and the need to create standardized communication materials that incorporate input from multiple stakeholders. Moreover, the paper highlights the importance of making available autopayment options and fostering ongoing dialogue to address implementation challenges and make adjustments. It stresses the need to allocate appropriate resources for implementation and incorporate diverse stakeholder perspectives throughout the process. Additionally, the key takeaways note concerns related to utilization management, year-round opt-in availability, , and potential unintended consequences of the OOP cap.
The Alliance will continue to work with CMS on the implementation of the annual cap and payment installment policies, as well as provide educational materials for beneficiaries as additional details emerge.
To review the roundtable summary and recommendations, click here.
