Mental Health
More than 20 percent of older adults aged 60 and over suffer from a mental or neurological disorder. The most common neuropsychiatric conditions are dementia and depression, according to the World Health Organization. Substance-use disorders related to use of alcohol, illicit drugs, and prescription medications are increasing in prevalence among older adults, along with chronic pain issues that may complicate treatment access.
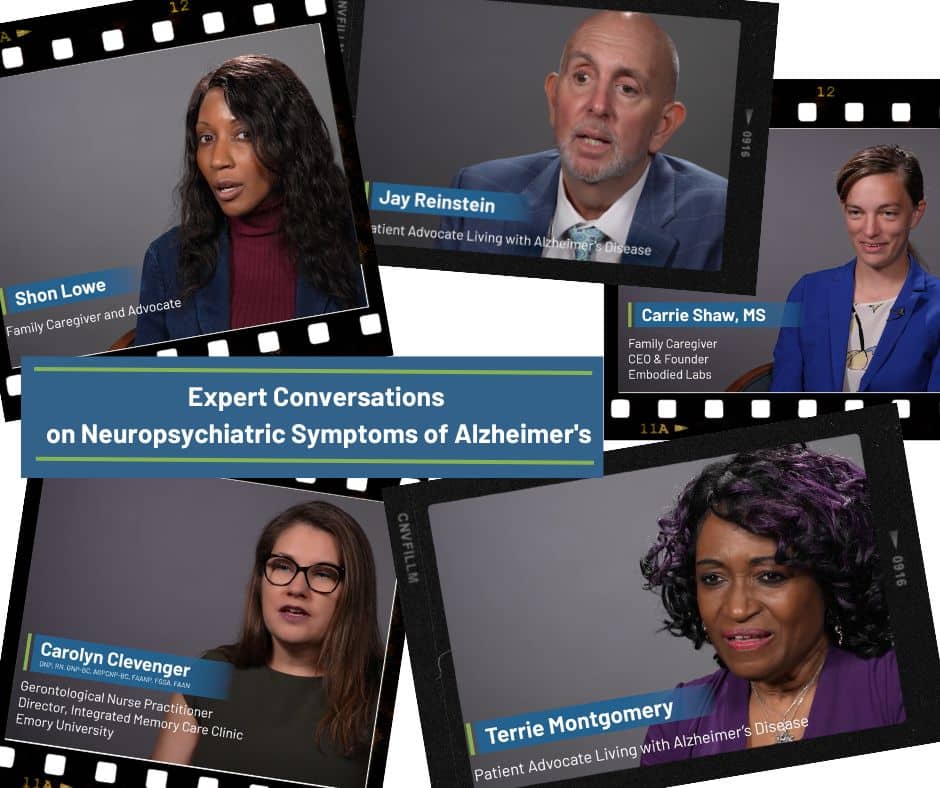
Individuals with Alzheimer’s disease (AD) and other dementias are often not diagnosed, despite numerous benefits of early detection including time to explore treatment options and clinical trials, establish a care plan, develop support networks, and plan for the future. As their disease progresses, these patients experience changes in how they communicate as well as significant behavioral changes that can cause depression, anxiety, agitation, apathy, psychosis, and other neuropsychiatric symptoms.
Close to 20 million adults in the U.S. had at least one depressive disorder in 2019 and its toll can be enormous—interrupting a person’s daily life, causing insomnia and fatigue, impacting memory and decision-making, raising the risk of cardiovascular disease, increasing pain sensitivity, weakening the immune system, causing weight changes, and raising the risk of death. Death by suicide is a serious problem for people ages 65 and older who make up 16 percent of the population but account for more than 19 percent of suicides.
While substance use disorders (SUDs) become less common with age, over one million adults ages 65 and older in the U.S. are estimated to live with a substance use disorder. SUDs can lead to serious illness, worsen existing medical conditions, harm mental health, impact relationships and well-being, increase healthcare usage, and even lead to death. SUDs in older adults are under-diagnosed and under-treated, despite the fact that as we age, our bodies and brains become more vulnerable to the potential harmful effects of these substances.
Mental illness can present differently in older adults — complicating timely recognition and treatment. In addition to the need for timely detection and treatment, clinical encounters with these patients often involve difficult conversations and the Alliance has created a series of tip sheets for clinicians and caregivers with ideas on how to have these important conversations:
Alzheimer’s Disease & Related Dementias
Depression & Suicide in Older Adults
Substance Use Disorders & Mental Health
The Healthy Aging Blog
Videos

Webinar: Financing the Cure: Exploring the Ecosystem of Alzheimer’s Disease Research Funding
The Accelerate Cures/Treatments for All Dementias (ACT-AD) held a webinar on July 13, 2021 for an in-depth…
more.
Webinar: Research and Clinical Development in Lewy Body Dementia
On December 7, 2020, ACT-AD held a webinar on cutting-edge research on Lewy Body dementia (LBD). The webinar…
more.
Webinar: The Emerging Antimicrobial Protection Hypothesis of Alzheimer’s Disease
The Accelerate Cure/Treatments for Alzheimer’s Disease (ACT-AD) Coalition held an educational webinar on April 18, 2019 on…
more.